Lung Clots From Coronavirus
The COVID-19 infection was classified from the beginning as a flu picture that could be complicated by pneumonia. However, recent findings raised the presence of clots in the lungs of coronavirus patients who had died.
These autopsies called into question what was considered the regular mechanism of evolution of the infection. It could be that pulmonary embolism ended up being the cause of death in some cases, and not sepsis from pneumonia.
Although we continue talking about the thoracic area, two different systems are involved depending on whether they are alveoli with pus or blood vessels with clots. In pneumonia we focus on the respiratory system, while pulmonary embolism has a strong component of the circulatory system.
Clots in the lungs are capable of obstructing the circulation of blood in the lung tissue, which would prevent the oxygen that enters through inspiration from passing to the other tissues. In the short term, tissues without oxygen die.
This led to the development of intensive therapy care protocols for patients with COVID-19, which involve the use of anticoagulants if certain criteria are met. Anticoagulants are drugs that stop the process of thrombus and emboli formation. However, they cannot be used without precautions, since the adverse effect is bleeding.
The discovery of clots in the lungs
A study published recently in the medical journal Radiology analyzed X-rays and some laboratory parameters of patients with COVID-19 pneumonia. Based on their findings, people began to speak more strongly about clots in the lungs due to coronavirus.
The researchers detected that more than 20% of those infected with coronavirus had signs of pulmonary embolism in their chest CT scans. And the average appearance of said embolism was 12 days after being diagnosed.
If the presence of pulmonary embolism in these patients is compared with others who are not positive for COVID-19, it is evident that the proportion is higher. In critically ill individuals from any cause, up to 1% develop pulmonary embolism, but if we only look at those infected with coronavirus, that value rises to almost 10%.
A substance that is measured in the blood and that is indicative of coagulative processes is D-dimer. This substance was also found to be higher in patients with SARS-CoV-2 than in the rest of the inpatient population.
High levels of D-dimer correspond to the high incidence of thrombotic events. That is, if the D-dimer is high in the blood, these people are at greater risk of developing clots that lead to pulmonary embolism.

Clots in the lungs are unable to carry oxygen
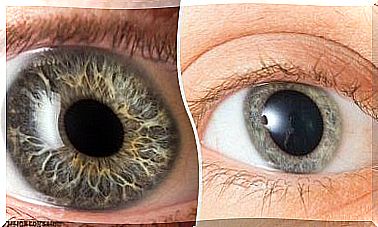
As some scientific studies well explain, clots in the lungs of coronavirus patients seem more like a circulatory problem than a respiratory problem. When circulation is obstructed, the rest of the tissues are left without oxygen.
Some series of patients have had relatively good respiratory outcomes. This means that their breathing mechanics were not altered to the point that oxygen could not enter the body. The problem was, then, the oxygen couldn’t reach the other vital tissues, like the heart and brain.
If oxygen does not circulate, more than sepsis we should speak of hypoxia. Sepsis is the spread of an infection throughout the rest of the body, starting from a specific point – the lungs, for example. Instead, hypoxia is the low concentration of available oxygen.
Our cells need oxygen to function. The metabolism and the actions that generate internal energy depend on a good oxygen supply. The clearest example may be that of exercise, when the muscles request more oxygen from us and we accelerate breathing.

Can it be detected in time?
Fortunately, scientific advances serve to improve care protocols. At present, intensive care units are implementing methods to diagnose clotting problems early in patients with coronavirus.
Both exaggerated clotting and bleeding are dangerous. There are management plans for each of these situations, always considering the adverse effects that exist in each patient, according to their comorbidities and their general clinical condition.
What should I do as a patient?
In itself, this issue of coronavirus clots in the lungs is the exclusive competence of treating physicians. There are no specific symptoms that alert a specific person about this process, since the reasons for consultation remain the same:
- Fever
- Decay
- Cough and shortness of breath
Yes, it is a priority to consult when these signs appear. Early detection reduces the risks of progressing to the most serious forms of COVID-19, such as pneumonia and pulmonary embolism.